Cerezyme (imiglucerase) for Gaucher disease
What is Cerezyme for Gaucher disease?
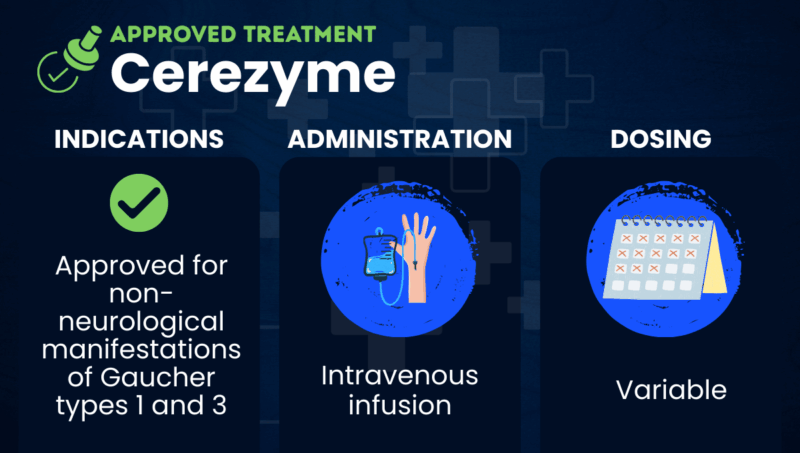
Cerezyme (imiglucerase) is an enzyme replacement therapy (ERT) approved for non-neurological symptoms of Gaucher disease type 1 or type 3, meaning symptoms that occur outside the brain and spinal cord.
Gaucher disease is caused by genetic mutations that lead to a deficiency of the glucocerebrosidase (GCase) enzyme. As a result, certain fatty substances can build up in the body and cause a range of symptoms. Some forms of the disease can also affect the central nervous system (CNS), which includes the brain and spinal cord.
Like other ERTs, Cerezyme provides a functional, lab-made version of GCase to help break down this buildup. While it can improve several non-neurological symptoms, it is generally not effective for symptoms affecting the CNS.
Cerezyme is given as an intravenous (into-the-vein) infusion and is marketed by Sanofi. In 2026, it became the first therapy approved in the U.S. for Gaucher disease type 3.
Therapy snapshot
| Brand name: | Cerezyme |
| Chemical name: | Imiglucerase |
| Usage: | Used to treat non-CNS manifestations of Gaucher disease types 1 and 3 |
| Administration: | Intravenous infusion |
Who can take Cerezyme?
In the U.S., Cerezyme is approved to treat non-CNS disease manifestations in adults and children with type 1 or type 3 Gaucher disease.
In the European Union and Canada, Cerezyme is approved for people with type 1 and type 3 Gaucher disease who have at least one of the following non-neurological symptoms:
- an enlarged liver or spleen
- bone disease
- anemia (low levels of healthy red blood cells)
- low platelet counts (platelets help blood clot)
There are no known contraindications for using Cerezyme. However, it has a boxed warning that it could cause exaggerated immune reactions (hypersensitivity), including a life-threatening systemic reaction called anaphylaxis, which may require stopping treatment in some cases.
How is Cerezyme administered?
Cerezyme is given by intravenous infusion. Infusions should be administered by a healthcare provider with the training and equipment needed to manage hypersensitivity reactions. Infusions usually take about one to two hours, but they may take longer in people who have had infusion-related reactions in the past.
The recommended dose ranges from 2.5 units/kg three times a week to 60 units/kg once every two weeks. A healthcare provider will choose the best dosing schedule based on disease severity and treatment goals.
If someone has had hypersensitivity reactions before, their healthcare provider may recommend premedication, such as antihistamines or corticosteroids, before the infusion.
Cerezyme in Gaucher clinical trials
The U.S. approvals of Cerezyme were largely supported by data from three clinical studies.
- A Phase 3 trial, RC 91-0110, enrolled 30 people with Gaucher disease type 1, ages 12 to 69. Participants received Cerezyme or its predecessor, Ceredase (alglucerase), at a weight-based dose once every two weeks for about six months. Results showed that Cerezyme and Ceredase had comparable efficacy in reducing liver and spleen volume and in improving blood-related measures. Most people receiving Cerezyme also showed improvements in bone-related outcomes.
- In an extension study for RC 91-0110, participants could continue their assigned treatment for an additional three months. After that, all participants could receive Cerezyme for 15 more months. The medication demonstrated sustained efficacy for up to two years.
- An observational study (NCT00358943) from the International Collaborative Gaucher Group included more than 1,000 children and adults with Gaucher disease type 1 and about 100 with Gaucher disease type 3 who were treated with Cerezyme. After about two years, participants showed reductions in spleen and liver volume and increases in red blood cell and platelet levels. Children in the study also showed improved growth, which can be stunted in Gaucher disease.
Cerezyme side effects
The most common side effects reported with Cerezyme include:
- back pain
- chills
- dizziness
- fatigue
- headache
- allergic reactions
- nausea
- fever
- vomiting
According to the boxed warning on Cerezyme’s label, treatment should be started in a healthcare setting with appropriate staff and equipment available to manage any hypersensitivity reactions. Signs of a hypersensitivity reaction may include itching, skin redness, hives, swelling under the skin, chest discomfort, shortness of breath, cough, bluish discoloration of the skin, fast heartbeat, or low blood pressure.
Reactions at the infusion site are also possible and may include swelling, itchiness, rash, hives, burning sensations, discomfort, chills, fatigue, fever, and high blood pressure.
If severe hypersensitivity or infusion-site reactions occur, Cerezyme should be discontinued, and medical treatment should be started immediately.
In some cases, a patient may be able to restart treatment later using a lower infusion rate or with medicines to help prevent future reactions. After a severe reaction, patients and providers should weigh the potential risks and benefits of re-administering Cerezyme.
Gaucher Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

