VPRIV (velaglucerase alfa) for Gaucher disease
Last updated April 4, 2025, by Inês Martins, PhD

What is VPRIV for Gaucher disease?
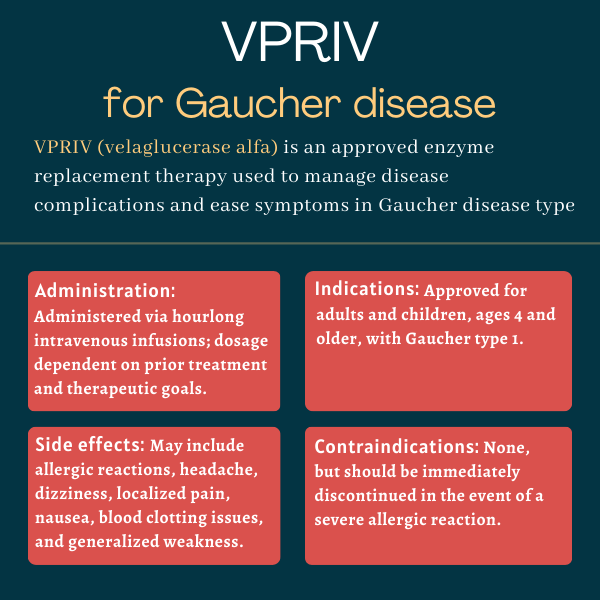
VPRIV (velaglucerase alfa) is an enzyme replacement therapy (ERT) approved as a long-term treatment for people with Gaucher disease type 1.
The therapy is designed to deliver the enzyme that’s lacking in Gaucher patients. It was proven safe and effective at managing certain disease complications and easing symptoms in both adult and pediatric patients, ages 4 and older.
Administered via intravenous, or into-the-vein, infusions, VPRIV is manufactured and marketed by Takeda Pharmaceuticals.
Therapy snapshot
| Brand name: | VPRIV |
| Chemical name: | Velaglucerase alfa |
| Usage: | Used to manage disease complications and ease symptoms of Gaucher type 1 |
| Administration: | Intravenous infusion |
How does VPRIV work?
An inherited disease, Gaucher is caused by mutations in the GBA1 gene, which provides instructions for making glucocerebrosidase — an enzyme responsible for breaking down a fatty molecule with the similar-sound name glucocerebroside.
Because people with Gaucher cannot make enough working glucocerebrosidase, glucocerebroside accumulates to toxic levels in certain cells, mainly in immune cells called macrophages, causing damage in several tissues and organs.
Gaucher disease type 1 is the most common form of the condition in North America and Europe. This form of the disease does not affect the brain or spinal cord and its symptoms can start anytime between childhood and adulthood. Symptoms and complications of this form include reduced levels of red blood cells and platelets, which are cell fragments involved in blood clotting, an enlarged spleen and liver, and bone problems.
VPRIV is an ERT designed to supplement the missing or deficient glucocerebrosidase in Gaucher patients. Administered intravenously, the enzyme travels through the bloodstream to affected cells, where it is absorbed and helps break down excess glucocerebroside.
The delivered enzyme, velaglucerase alfa, is produced using gene activation technology in lab-grown human cells. This technology, as its name suggests, activates the native GBA1 gene in the cells, and enables them to produce large amounts of the enzyme.
Velaglucerase alfa has the same sequence as the naturally occurring human glucocerebrosidase, but it undergoes specific modifications during cell culture, namely the addition of certain sugar molecules at specific protein regions. These modifications help optimize the enzyme’s entry into macrophages.
Who can take VPRIV?
VPRIV was approved by the U.S. Food and Drug Administration in February 2010 for the long-term treatment of children and adults with type 1 Gaucher disease.
Later that year, the therapy was also cleared in Canada and the European Union for the same indication.
Who should not take VPRIV?
The prescribing information for VPRIV does not list any contraindications, or reasons why the therapy should not be used.
However, it contains a boxed warning for potentially life-threatening allergic reactions, including anaphylaxis, to the medication. Such reactions have been reported in some patients early in the course of treatment or after prolonged therapy.
VPRIV should be administered in a healthcare setting with appropriate medical monitoring and emergency support. If a severe allergic reaction occurs, treatment should be discontinued, and appropriate medical intervention, including the use of epinephrine (the active ingredient in an EpiPen), should be immediately initiated.
How is VPRIV administered?
VPRIV is given by a healthcare professional as an hourlong intravenous infusion, once every two weeks, at a dosage that depends on the patient’s prior treatment history and therapeutic goals.
For patients ages 4 and older who have never received an ERT, VPRIV’s recommended starting dose is 60 units per kg of body weight (U/kg), once every two weeks. Those receiving a stable dose of Cerezyme (imiglucerase) — an older ERT for Gaucher type 1 — can switch to VPRIV, at the same dose as their previous Cerezyme dose, two weeks after their last Cerezyme infusion.
In both patient groups, the dosage may subsequently be adjusted based on the individual patient’s response to treatment.
VPRIV is available as single-dose vials containing 400 units of velaglucerase alfa as a sterile white to off-white powder, which must be diluted in 4.3 mL of sterile water. The appropriate dose is then diluted into a saline solution to a final volume of 100 mL.
Because VPRIV may cause severe allergic reactions, it must be administered under the supervision of a healthcare provider trained in managing these reactions. Infusions also should take place in a healthcare setting with appropriate medical monitoring and emergency support, including access to cardiopulmonary resuscitation equipment. If a severe allergic reaction occurs, the infusion should be immediately stopped and the patient should receive prompt medical treatment.
VPRIV in Gaucher clinical trials
VPRIV’s approval was largely supported by data from three late-stage clinical trials involving 99 adults and children with Gaucher type 1.
Two Phase 3 trials — Study 032 (NCT00430625) and Study 039 (NCT00553631) — enrolled patients who were not on any form of Gaucher treatment. Another Phase 2/3 trial, meanwhile, called Study 034 (NCT00478647), involved participants who were receiving Cerezyme immediately before starting VPRIV.
Study 032
Study 032 enrolled 25 patients, ages 4 and older, who had not received Gaucher-specific treatment for at least 30 months, or 2.5 years, before entering the study. All had Gaucher-related anemia — low levels of red blood cells, or of the oxygen-transporting protein hemoglobin — and either low platelet counts, called thrombocytopenia, an enlarged liver, or an enlarged spleen.
The participants were randomly assigned to receive VPRIV at a dose of either 45 or 60 U/kg, given every other week for one year. The main goal was to assess changes in blood hemoglobin levels after one year of treatment with the high dose. Secondary measures included changes in hemoglobin levels with the low dose, as well as changes in platelet counts and spleen and liver volume with either dose.
The results showed that the trial met its main goal, with the now recommended dose for previously untreated patients leading to a significant increase, by 23.3%, in hemoglobin levels from study’s start, or baseline. That increase was considered clinically meaningful.
The 60 U/kg dose also significantly increased, by 65.9%, blood platelet levels, and significantly reduced, by 50.4%, spleen volume. Reductions in liver volume also were seen after one year of treatment, but these failed to reach statistical significance after adjusting for other factors.
Study 039
The head-to-head Study 039 compared the 60 U/kg dose of VPRIV against Cerezyme in patients who had not received any approved or experimental Gaucher treatment for at least one year prior. As in the previous trial, eligible participants were required to have anemia and either thrombocytopenia or enlarged organs.
A total of 34 individuals, ages 4 and older, were randomly assigned to receive either VRPIV or Cerezyme, given as an hourlong infusion once every two weeks for nine months. The goal was to determine whether VPRIV was at least non-inferior to Cerezyme at lessening disease signs and symptoms.
No significant group differences were seen in terms of outcomes after nine months of treatment. The results showed the two therapies led to similar increases in hemoglobin and platelet levels, and to similar reductions in spleen and liver volumes.
Study 034
Study 034 enrolled 40 patients, ages 9 and older, who had been receiving Cerezyme treatment at doses ranging between 15-60 U/kg, given every other week, for at least 30 consecutive months. These patients also were required to be on a stable dose for at least six months.
Upon entering the trial, participants stopped Cerezyme and switched to a similar dose of VPRIV, once every week, for one year, starting 14 to 30 days after their last Cerezyme infusion. Dose increases up to 60 U/kg were allowed if patients experienced worsening in disease parameters.
The trial met its primary goal of showing that switching to VPRIV was safe and well tolerated in individuals previously given Cerezyme. Additionally, hemoglobin and platelet levels remained generally stable, and no significant differences were observed in spleen and liver volume relative to the study start, meeting the study’s secondary goals.
Long-term extension Study 044
A total of 95 patients from the previous trials opted to enter a long-term extension Phase 3 study (NCT00635427), dubbed Study 044, in which all received every-other-week VPRIV infusions for up to five years.
Altogether, 57 individuals who had taken part in studies 032 and 039 enrolled in the extension. Each received 60 U/kg of VPRIV until completing a total of two years of VPRIV treatment across the main trial and the extension study. After two years, dose adjustments by 15 U/kg were allowed every 12 months, or at each one-year mark, provided the dose stayed within the 15-60 U/kg range.
Data indicated that VPRIV continued to be safe and well tolerated with longer treatment. Significant improvements also were seen in all disease parameters in the first two years of VPRIV treatment — including in patients who were first treated with Cerezyme for nine months in Study 039 and then switched to VPRIV in the extension study.
Observed improvements were either maintained or continued at a slower rate over the following years.
The 38 participants who crossed over from Study 034 to the extension study were treated with the same VPRIV dose they had been receiving in the main trial. These patients were followed for up to 50 months, or slightly longer than four years, in the extension study, with total treatment for up to five years of follow-up from the Study 034 start.
Dose adjustments were also allowed every 12 months, and 10 adults required at least one 15 U/kg-dose increase in the extension study, the data showed.
Long-term VPRIV treatment after Cerezyme was found to be generally safe and well tolerated, without reports of serious adverse events related to VPRIV, the results showed.
Also, hemoglobin and platelet levels, as well as spleen and liver volumes, remained generally unchanged over the five years of follow-up. Blood levels of chitotriosidase and CCL18, two biomarkers of Gaucher burden, declined over time in nearly all patients.
Common side effects of VPRIV
The most common side effects of VPRIV reported in clinical trials were:
- allergic reactions
- headache
- dizziness
- abdominal pain
- nausea
- back pain
- joint pain
- blood clotting issues
- fatigue or generalized weakness
- fever.
The therapy’s safety profile was similar between pediatric patients — those ages 4 to 17 — and adults. Still, available data showed certain side effects were more commonly reported in children relative to adults. These included rash, blood clotting problems, and fever.
Allergic reactions
VPRIV carries a boxed warning noting that its use may lead to life-threatening allergic reactions, including anaphylaxis. Such events have been reported both early in the treatment course and after extended therapy duration.
Allergic reactions were the most frequently observed side effects among VPRIV-treated patients in trials, though they were generally mild in severity. The most common symptoms were headache, dizziness, nausea, fatigue, fever, and blood pressure outside the normal range. Among patients who had not received previous treatment, allergic reactions occurred most frequently within the first six months of VPRIV treatment, with their frequency tending to decrease over time.
After the therapy was approved, certain additional allergic reactions were reported. Among them were symptoms such as chest discomfort, shortness of breath, itching, and vomiting.
VPRIV should only be administered under the supervision of a healthcare provider experienced in managing allergic reactions, including anaphylaxis. Treatment should be started in a healthcare facility equipped with appropriate medical monitoring and support measures, such as emergency resuscitation equipment.
Patients should be educated about the symptoms of anaphylaxis or other life-threatening allergic reactions, and should be instructed to seek immediate medical care if these symptoms develop.
Treatment of these reactions depends on their severity. This may involve slowing the infusion rate, temporarily stopping the infusion, or administering antihistamines, corticosteroids, and/or fever-reducing medications. In cases of severe allergic reactions, VPRIV should be discontinued, and appropriate medical treatment immediately started.
For patients who have experienced allergic reactions during prior VPRIV infusions, premedication with antihistamines and/or corticosteroids may be considered to prevent future reactions.
Use in pregnancy and breastfeeding
Available data from more than 300 pregnancies do not suggest an increased risk of major birth defects, miscarriage, or other adverse maternal and fetal outcomes with VPRIV treatment.
In animal studies, exposure to the therapy during pregnancy at doses greater than those recommended for people was not associated with signs of fetal harm.
Still, pregnancy may worsen Gaucher type 1 symptoms or result in new symptoms. If disease symptoms are not well-controlled before and during pregnancy, patients may develop complications that interfere with normal fetal development and have an increased risk of miscarriage.
Whether VPRIV can be found in human breast milk and whether it affects nursing infants or breast milk production remains unclear. However, the naturally occurring glucocerebrosidase enzyme is known to be excreted in breast milk. Patients considering breastfeeding should weigh the potential benefits of VPRIV treatment against any possible risks to their infant from either the medication or their underlying condition.
Gaucher Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- A holistic approach to healthcare helps me live well with Gaucher
- Elevated uric acid levels linked to disease severity in type 1 Gaucher
- Abcertin meets Cerezyme biosimilar criteria in Phase 1 study
- Gaucher disease diagnosis speeds up, but complications still common
- A week in the life of a working mom, wife, and caregiver
Related articles