Fatty Liver Common, Linked to Scarring, in Type 1 Gaucher, Study Finds
Liver steatosis, a condition characterized by the buildup of fatty tissue inside the liver, is common in adults with type 1 Gaucher disease and is strongly associated with metabolic changes linked to fatty liver disease, an Italian study has found.
The condition is also associated with liver scarring (fibrosis) among those using enzyme replacement therapy (ERT).
The study, “Liver steatosis is highly prevalent and is associated with metabolic risk factors and liver fibrosis in adult patients with type 1 Gaucher disease,” was published in the journal Liver International.
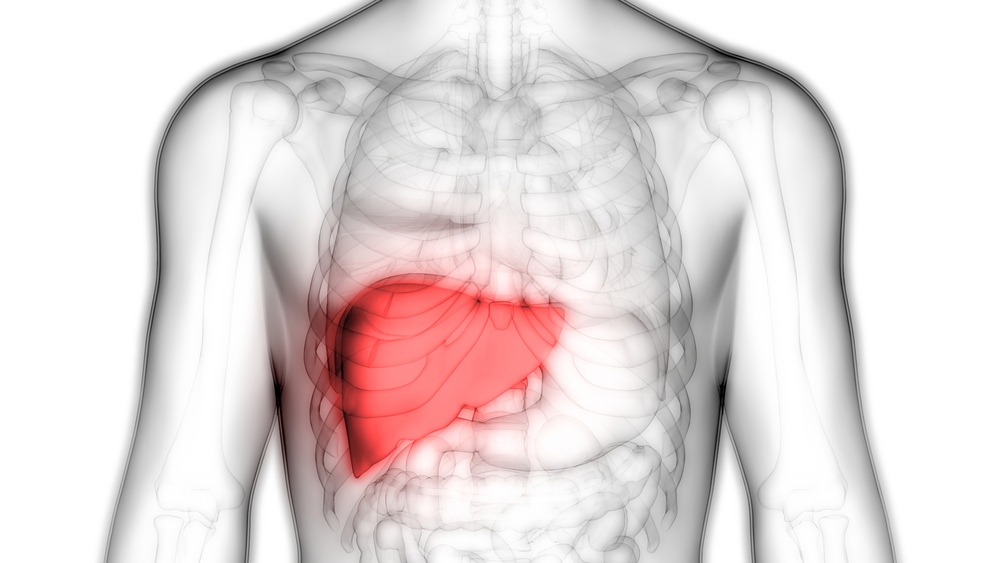
Type 1 Gaucher, the most common form of this disease, is caused by mutations in the GBA gene that affect the production of an enzyme called beta-glucocerebrosidase. This enzyme lack leads to a fatty substance called glucocerebroside accumulating in immune cells, which then infiltrate different organs and tissues — particularly the liver and spleen — causing them to enlarge, a condition known as hepatosplenomegaly.
“Liver involvement in type 1 GD [Gaucher disease] is almost universal and ranges from hepatomegaly, with or without liver enzymes alterations, to liver fibrosis, cirrhosis, portal hypertension [high blood pressure in the portal vein] and hepatocellular carcinoma,” the investigators wrote.
ERT, a form of therapy that involves providing patients with an artificial form of the enzyme beta-glucocerebrosidase, has shown effectiveness at alleviating most symptoms of Gaucher, as well as prolonging patients’ life expectancy and improving their quality of life. However, over time, the therapy may lead to excess weight.
The metabolic alterations that often accompany Gaucher, including insulin resistance and excessive levels of fatty molecules circulating in the blood (dyslipidemia) in combination with an increasingly unhealthy lifestyle, may cause patients to develop liver steatosis.
To assess the prevalence of liver steatosis and identify the risk factors that could prompt those with type 1 Gaucher to develop the condition, investigators at the University of Modena and Reggio Emilia and their colleagues reviewed clinical data from 20 adults with type 1 Gaucher who had been monitored between 2015 and 2017.
During the study, patients underwent vibration controlled transient elastography (VCTE) — a non-invasive technology that allows physicians to determine the stiffness of the liver — to assess the presence and/or severity of liver steatosis.
This was done by evaluating the controlled attenuation parameter (CAP), a VCTE measure of how much of the ultrasound waves produced by the Fibroscan device are deterred by the amount of fatty tissue in the liver.
Patients were considered to have liver steatosis when their CAP values were at least 250 decibels per minute (dB/min). From the 20 patients — 10 men and 10 women, with a median age of 48 years — 18 were receiving ERT, 16 of whom had been on a stable regimen for at least two years.
A significant proportion of participants had a series of metabolic alterations, which included high blood pressure (50%), excessive body weight (40%), insulin resistance (15%), and changes in blood sugar metabolism (10%).
In the overall study population, results showed that CAP values ranged from 165 to 358 dB/min, with eight individuals (40%) having values of at least 250 dB/min and thus qualifying for liver steatosis.
Statistical analyses found that liver steatosis was associated with several measures of fatty tissue accumulation, such as body weight, body mass index, and waist circumference, as well as high blood pressure, insulin resistance, and metabolic syndrome. Notably, metabolic syndrome comprises a series of conditions that increase a person’s risk of developing heart disease, stroke, or type 2 diabetes. In contrast, neither the dose nor the duration of ERT was associated with liver steatosis in these patients.
Yet, in the 16 participants who had been on a stable ERT regimen, high CAP values indicative of liver steatosis were found to be associated with stiffness and tissue scarring.
“Significant steatosis is highly prevalent in adult type 1 GD patients and is strongly associated with a worse metabolic profile, featuring metabolic dysfunction‐associated fatty liver disease (MAFLD),” the researchers wrote.



