Potential Targeted Therapy for Cancer Shows Promise for Gaucher Disease, Study Finds
Written by |
A targeted therapy currently being investigated for treating certain types of cancer can overcome some of the limitations of standard enzyme replacement therapy and be a promising therapeutic avenue for Gaucher disease and other lysosomal storage disorders, a study says.
The therapy, which uses small cellular carriers to deliver therapeutic agents to specific cells in the body, may even be useful to treat certain neurological disorders such as Parkinson’s disease, the investigators said.
The study, “Systemic enzyme delivery by blood-brain barrier-penetrating SapC-DOPS nanovesicles for treatment of neuronopathic Gaucher disease,” was published in the journal EBioMedicine.
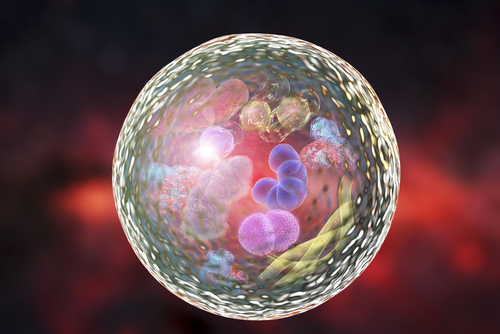
Gaucher disease is a lysosomal storage disorder caused by a mutation in the GBA gene, which impairs the production of beta-glucocerebrosidase. This enzyme is responsible for breaking down a fatty substance called glucocerebroside, and in its absence, glucocerebroside starts to accumulate inside immune cells called macrophages, which then become Gaucher cells.
Existing Gaucher treatments include enzyme replacement therapies (ERTs) and substrate reduction therapies (SRTs). ERTs use artificial enzymes meant to replace those missing in patients, while SRTs seek to prevent the body from producing the toxic substances that accumulate inside cells.
Despite being effective at easing some of the symptoms of Gaucher disease, these therapies fail to minimize the effects of the disease on the central nervous system (CNS, comprising the brain and spinal cord). This happens because the treatments are unable to cross the blood-brain barrier — a highly selective membrane that separates the brain from peripheral blood circulation — and reach the CNS.
Now, researchers at the University of Cincinnati may have found a way to overcome this limitation. Their idea consisted of using small cellular carriers called nanovesicles that are currently being assessed as delivery vectors for anti-cancer therapies.
“[Certain] nanovesicles have the ability to cross the blood-brain barrier and selectively target brain tissue, providing a biological vehicle for delivering the enzyme replacement therapy,” Xiaoyang Qi, PhD, the study’s senior author, said in a news story.
These nanovesicles, called SapC-DOPS, result from the combination of the protein saposin C (SapC) with the phospholipid dioleoylphos-phatidylserine (DOPS). SapC is a small protein found in lysosomes — the cell compartments responsible for digesting and recycling different types of molecules — that prevents beta-glucocerebrosidase from being destroyed, while also promoting its activity. Phospholipids are cell membrane components.
In prior studies, Qi and his team successfully used these nanovesicles in animal models to deliver cancer-killing agents to malignant cells in different organs, including the brain. In the new study, the scientists tested the nanovesicles’ potential to carry and deliver functional beta-glucocerebrosidase to CNS cells of a mouse model of Gaucher disease.
For all experiments, the investigators used velaglucerase alpha (brand name VPRIV), an ERT approved in the U.S. and E.U. for patients with type 1 Gaucher disease.
Experiments in a lab dish showed that compared to free beta-glucocerebrosidase, the enzyme incorporated into the SapC-DOPS nanovesicles was more stable, and easily taken up by the cells. As a result, cells initially unable to produce the enzyme by themselves started showing a high activity of beta-glucocerebrosidase.
When injected into mice engineered to mimic the symptoms of Gaucher, the nanovesicles carrying functional enzyme successfully crossed the blood-brain barrier, increased the activity of beta-glucocerebrosidase, and lowered the levels of glucocerebroside in the animals’ CNS. Treatment also reduced inflammation in the brain and alleviated some neurological symptoms.
The team also found that, to deliver the functional enzyme to cells in the CNS, the nanovesicles used a specific receptor and the lymphatic system, which is the network of vessels that transport lymphatic fluid and immune cells in and out of tissues.
“In this study, we showed that the nanovesicle was able to deliver the enzyme to the necessary tissues in animal models, especially the brain,” said Ying Sun, PhD, the study’s first author.
“This novel therapeutic approach corrects the deficiency of the enzyme in central nervous system cells and tissues and is efficient in reducing inflammation and neurological issues in animal models with [some types of] Gaucher disease,” Sun added.
The SapC-DOPS nanovesicles used in the study are biological products that meet guidelines for good manufacturing practices with excellent safety when tested in a Phase 1 trial (NCT02859857) in patients with advanced solid tumors, the researchers said.
“Although this study was focused on a rare disease, there may be implications for similar but vastly more common conditions such as Parkinson’s disease where decreased activity of the same enzyme have been documented in the patients’ brains,” Qi said. “This has the potential to improve patient care.”