Distinct Genetic Profiles in Single Family Illustrate Challenges to GD Diagnosis, Study Says
Written by |
Four distinct genetic profiles in Gaucher disease (GD) patients within a single family highlight the variability in disease severity and its difficult diagnosis, a study reports.
The study, “Comprehensive clinical, biochemical and genetic screening reveals four distinct GBA genotypes as underlying variable manifestation of Gaucher disease in a single family,” was published in the journal Molecular Genetics and Metabolism Reports.
GD is caused by mutations in the GBA gene, which provides instructions to produce an enzyme known as beta-glucocerebrosidase. Such defects lead to an altered enzyme and to the buildup of fatty substances (glucosylceramides) in macrophages, a type of white blood cell.
Signs, symptoms, age of onset, and severity of GD can vary widely, even within the same families and between identical twins. This makes the disorder difficult to identify, resulting in significant delays in diagnosis.
In the study, researchers described the case of a family in Albania, in which two generations experienced partially overlapping GD symptoms of variable severity.
After an original diagnosis of infection was ruled out, DNA samples from all family members were analyzed to better understand disease progression and variability.
The family, all diagnosed with GD type 1, consisted of seven members, four adults in the first generation and three youths in the second generation.
Two men and one woman (39–44 years old) of the first generation were siblings, all with severe forms of GD involving an enlarged liver and spleen, bone pain, and low platelet counts (thrombocytopenia). All of these patients had their spleens removed in their early 20s.
The fourth member of the first generation was a 43-year-old woman who married one of the affected siblings. She also had a milder form of GD with swelling in the liver and spleen, but no other symptoms.
All three family members of the second generation were the children of this couple: two boys, 18 and 15, and a girl, 8. The oldest boy, like his father, had a severe form of GD, while the younger boy and his sister had a milder form with enlarged spleens.
All patients, except for the 8-year-old girl, were receiving enzyme replacement therapy with VPRIV (velaglucerase alfa), marketed by Takeda.
Genetic analysis revealed that all three of the severely affected first-generation siblings had the same variants in one GBA copy. These alterations included a deletion in GBA (1265_1319del) that causes complete loss of enzyme function, and a missense mutation (259C > T) that may result in partially functional beta-glucocerebrosidase. Of note, missense variants refer to the change in one amino acid, the building blocks of proteins.
The fourth member of the first generation, the mother with milder GD, had the same missense mutation (1226A > G) in both GBA gene copies.
Among the second generation, the 18-year-old boy inherited the deletion mutation from his father and the missense mutation from his mother. While the other two children, both with mild forms of GD, inherited their two different missense mutations from each of their parents.
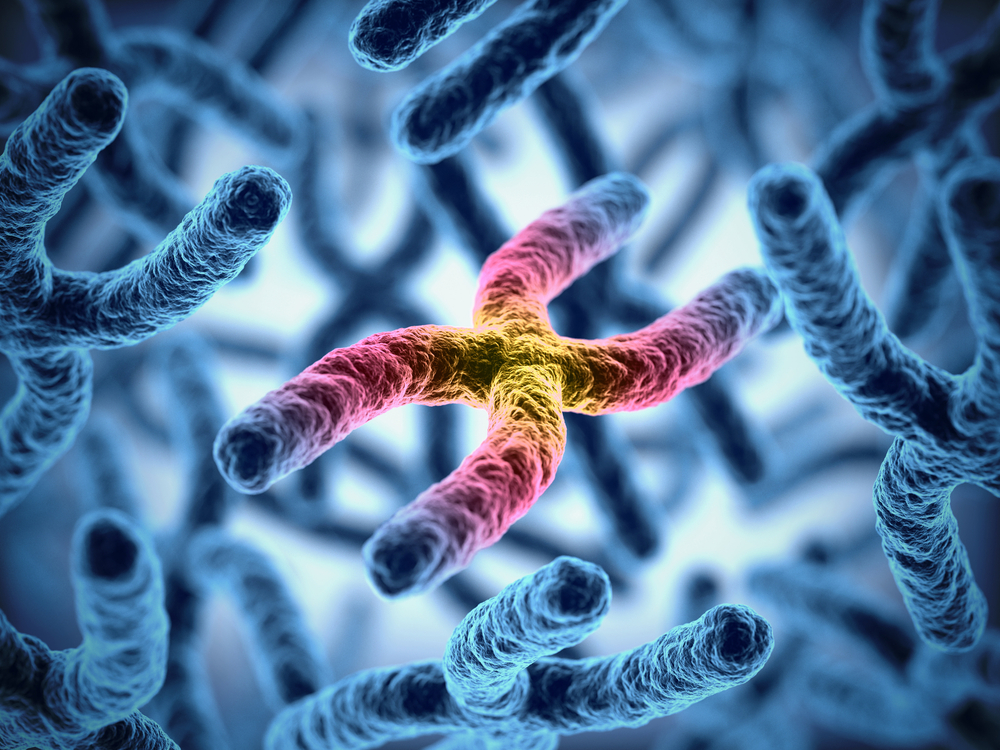
Family members with the deletion mutation (no functional enzyme) had greater disease severity than those with the missense variants only. Blood tests also showed that all family members with severe GD had abnormally high levels of lyso-Gb1 — a breakdown product of glucosylceramide and a marker of GD — compared to those with the milder forms.
Overall, this analysis identified four different genetic profiles within one family, which contributed to the variable symptoms and severity of GD among family members.
Typically, GD inheritance follows an autosomal recessive pattern — where a person inherits one mutated GBA gene copy from each parent, who carry one defective copy but are otherwise healthy. In this family, both parents had GD, which “adds further complexity,” the researchers wrote.
“The family thereby nicely exemplifies that, even in the presence of a positive family history, there are specific challenges for properly diagnosing GD,” they added.