Gaucher Disease May Rarely Include GI Symptoms, Case Report Highlights
Written by |
The case of a young women with Gaucher disease type 3, which affected her small bowel, calls attention to the possibility, although rare, that certain gastrointestinal (GI) symptoms can be a sign of Gaucher disease, a case report shows.
The patient presented with bowel obstruction and gastrointestinal bleeding, likely caused by the deposition of Gaucher cells and the development of a mass in her bowel.
The case report, “Small Bowel Mucosal Involvement and Mesenteric Mass Formation in a Young Female with Type 3 Gaucher Disease. A Case Report,” was published in the Journal of Gastrointestinal and Liver Diseases.
Gaucher disease is a condition caused by a deficiency in the glucocerebrosidase enzyme, which normally degrades a fat molecule called glucocerebroside. In Gaucher patients, this fat molecule accumulates in certain cells and causes some organs to function abnormally.
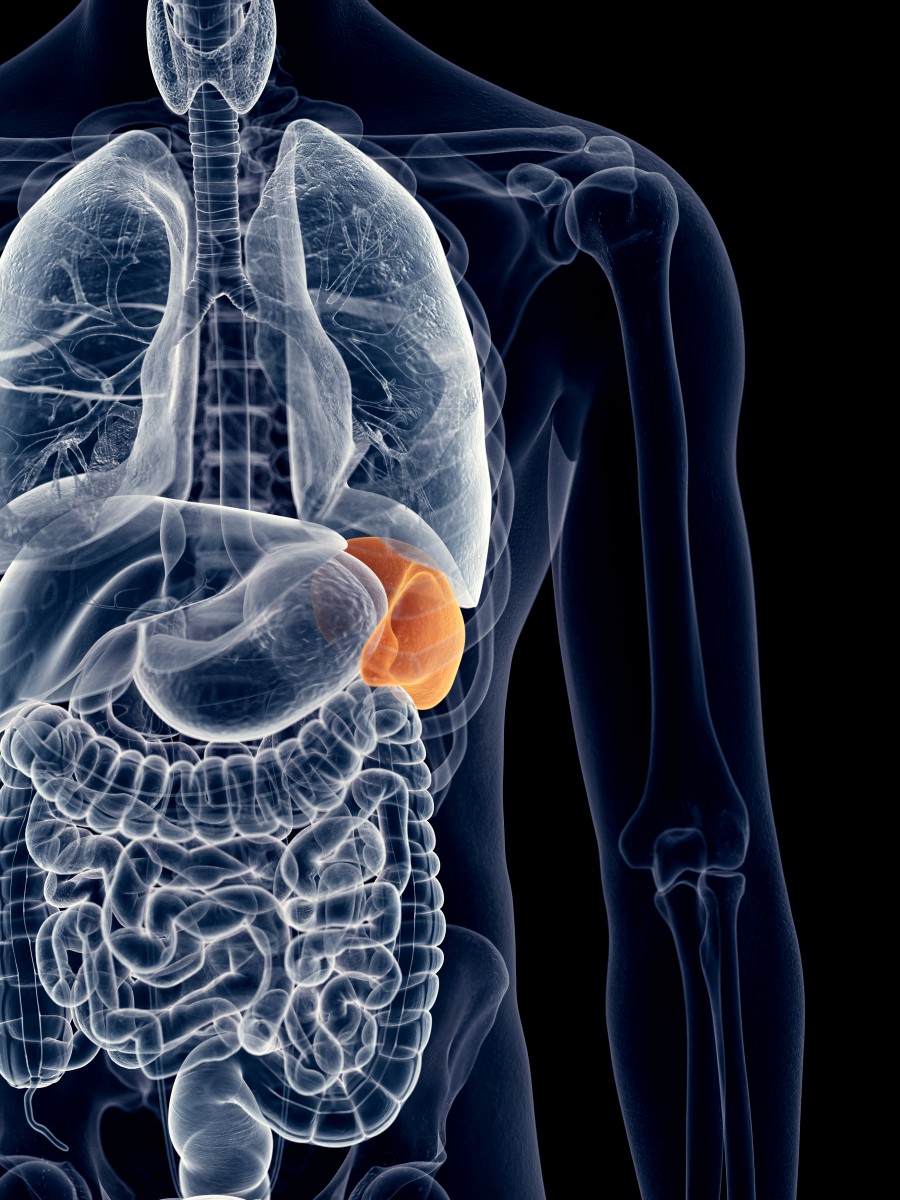
The condition mostly affects the spleen, liver, bone, and lungs, but other organs are sometimes also involved. In this case, researchers are reporting on a 24-year-old female who developed symptoms in her GI tract.
The patient had been diagnosed at 1 year old with Gaucher type 3, and had been receiving therapy with Cerezyme (imiglucerase) and albumin infusions, and Vimpat (lacosamide) and levetiracetam to control seizures.
She was admitted to the hospital due to pneumonia in February 2017, complaining of several GI symptoms. A computed tomography (CT) scan revealed enlargement of the liver and spleen, a typical sign of Gaucher disease, along with a mass in her abdomen.
Other observations included a thickening of the small bowel wall, enlargement of the colon, and dilated blood vessels at or surrounding the intestine, likely to be varices (abnormally dilated vessels).
She was discharged, but in June of the same year, she was hospitalized again with rectal bleeding, a high heart rate (tachycardia), low blood pressure, and anemia.
She was stabilized after a blood transfusion, and an additional CT exam confirmed the presence of varicose veins surrounding the intestine. She was discharged at the time.
In November, the patient returned to the hospital, with complaints of abdominal pain, intractable vomiting, and poor oral intake. Further exams revealed she had a small bowel obstruction, and a swollen small bowel and large bowel (colon), including a thickening of bowel loops.
Because of her abnormal blood levels, she was given a PEG tube, a feeding tube placed through the skin and the stomach wall. During the procedure, doctors noticed many white spots in her bowel, later seen by biopsy to contain many macrophages.
Macrophages overloaded with fatty materials (in this case, glucocerebroside) are a hallmark of Gaucher disease. It is this type of cell, called the Gaucher cell, that primarily accumulates in the tissues of people with this disorder.
The patient’s situation quickly deteriorated after the procedure, culminating in severe multi-organ failure and death.
Microscopic analysis of tissue samples at the time of her autopsy were consistent with the presence of Gaucher cells within the mass in the patient’s bowel. Marks suggestive of a GI bleed were also seen.
The brain also showed signs of deterioration due to the disease.
It is likely, the researchers propose, that the small bowel thickening, caused by Gaucher cell deposition, together with the accumulated mass, precipitated the bowel obstruction and GI bleeding.
These symptoms, rarely seen in Gaucher patients, “are complications that are more likely to be seen in long-standing, moderate-severe cases,” they said.
With the appearance of better therapies, such as enzyme replacement therapy, and current research efforts focused on the genetic causes of the disease, “it is possible that involvement of unusual locations and such complications become increasingly common,” according to the researchers.
“Treating clinicians should be cognizant of unexpected complications and quick to consider how they may relate to the underlying disease process,” they said.