Why do some Gaucher patients face Parkinson’s disease risk?
Researchers study sibling differences to pinpoint risk factors
Written by |
Differences in nerve cell function may explain why some people with Gaucher disease develop the neurodegenerative Parkinson’s disease and others do not, a study found.
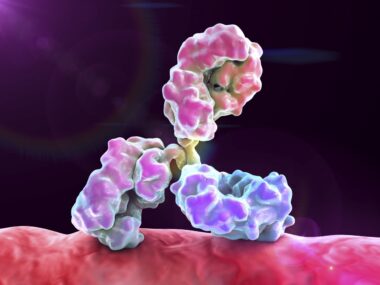
When researchers compared nerve cells derived from siblings with Gaucher with different outcomes — one developed Parkinson’s while the other did not — they found differences in certain protein levels and the function of synapses, the junctions through which nerve cells communicate.
The study, “Evaluation of Induced Pluripotent Stem Cell-Derived Dopaminergic Neurons from Siblings with Gaucher Disease Discordant for Parkinsonism,” was published in Movement Disorders.
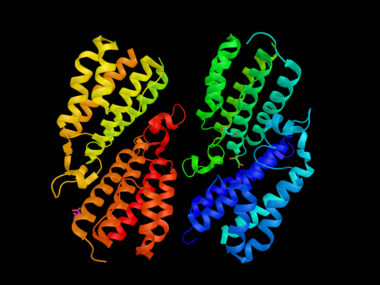
Gaucher is caused when mutations in the GBA1 gene lead to a dysfunctional or missing glucocerebrosidase (GCase), an enzyme that is needed to break down certain fatty molecules inside cells. Without a functional GCase, these molecules accumulate inside lysosomes, the cell’s recycling centers, causing damage to organs and tissues.
GBA1 mutations are also a genetic risk factor for Parkinson’s, a disorder marked by the progressive loss of dopaminergic neurons — nerve cells that produce dopamine, a brain signaling molecule involved in movement. A lack of dopamine signaling gives rise to hallmark motor symptoms of Parkinson’s, such as tremor, abnormally slow movements, and rigidity.
Most Gaucher patients don’t develop Parkinson’s
About 90% of Gaucher patients never develop Parkinson’s, and it’s not known why some people will develop the condition and others will remain unaffected.
A research team at the National Institutes of Health examined dopaminergic neurons derived from siblings with Gaucher to determine why one developed Parkinson’s and the other did not. This phenomenon is known as discordance, where two siblings carry the same mutations but only one develops a disease.
In one family, two brothers carried the same GBA1 mutations. The older brother was diagnosed with Gaucher at age 49 and began enzyme replacement therapy (ERT), which stabilized his clinical course. He was free of Parkinson’s at 73.
His younger brother was diagnosed with Gaucher at 47, remained untreated, and developed Parkinson’s at 52. He progressed to motor complications, psychiatric problems, and dementia, and died at 71.
Two sisters in another family carried the same GBA1 mutations. The older sister was diagnosed with Gaucher at 12, received ERT, and never developed Parkinson’s. She died at 63 from bone cancer. Her younger sister was diagnosed with Gaucher at age 8, and developed Parkinson’s at 55. Their unaffected middle sister carried no GBA1 mutations or Parkinson’s signs.
An examination of derived dopaminergic neurons revealed lower GCase protein levels in both brothers, and in both sisters with Gaucher compared with the unaffected sister.
There were no substantial differences in GCase levels between the Gaucher siblings with and without Parkinson’s in each family, “suggesting that the GBA1 genotype has a more substantial impact on GCase levels than [Parkinson’s] status,” the team wrote.
GCase activity was low in Gaucher patients, but did not correlate with Parkinson’s status. The fatty molecules that GCase acts upon (substrates), which build up in Gaucher, were similarly elevated in the siblings with Gaucher, regardless of their Parkinson’s status.
Because the growth of patient-derived neurons can be highly variable, the team examined only cells that produce tyrosine hydroxylase (TH), indicating correctly functioning dopaminergic neurons. TH is an enzyme that promotes the generation of L-DOPA, a precursor of dopamine.
Tests showed that GCase levels in the TH-producing dopaminergic neurons from the Gaucher sisters remained similar and were considerably lower than in the unaffected sister. There were also no differences in the levels of alpha-synuclein, a protein implicated in the loss of dopaminergic neurons in Parkinson’s.
The team found that in neurons from the Gaucher sisters, 80 proteins were increased and 118 proteins were decreased compared with those of their unaffected sister. The majority seemed to be related to lysosomal changes related to Gaucher.
Dopaminergic neurons from the younger sister who developed Parkinson’s showed an increase in chaperones, a class of proteins that help other proteins fold into their correct shape. This finding may reflect disruptions in proteins, potentially contributing to Parkinson’s, the team noted.
Other major differences between cells from the sisters with and without Parkinson’s involved the assembly and function of synapses.
Because dopaminergic neurons from Gaucher patients with and without Parkinson’s had similar GCase and fatty molecule levels, “neither explains the [Parkinson’s] discordance in the siblings, implicating genetic modifiers acting through other pathways,” the researchers wrote.
“An improved understanding of these genetic modifiers is critical for identifying individuals with GBA1 variants who may benefit from enhanced [Parkinson’s] monitoring and early clinical intervention,” they concluded.