Gaucher Patients Should Be Monitored Carefully for Bone Health, Case Report Suggests
Written by |
Enzyme replacement therapy (ERT) has limited effectiveness in addressing bone-related symptoms in Gaucher disease, namely the death of bone tissue due to loss of blood supply, a case study shows. The findings suggest that bone health should be closely monitored in these patients.
The study, “Bone manifestations in neuronopathic Gaucher disease while receiving high-dose enzyme replacement therapy,” was published in the journal Molecular Genetics and Metabolism.
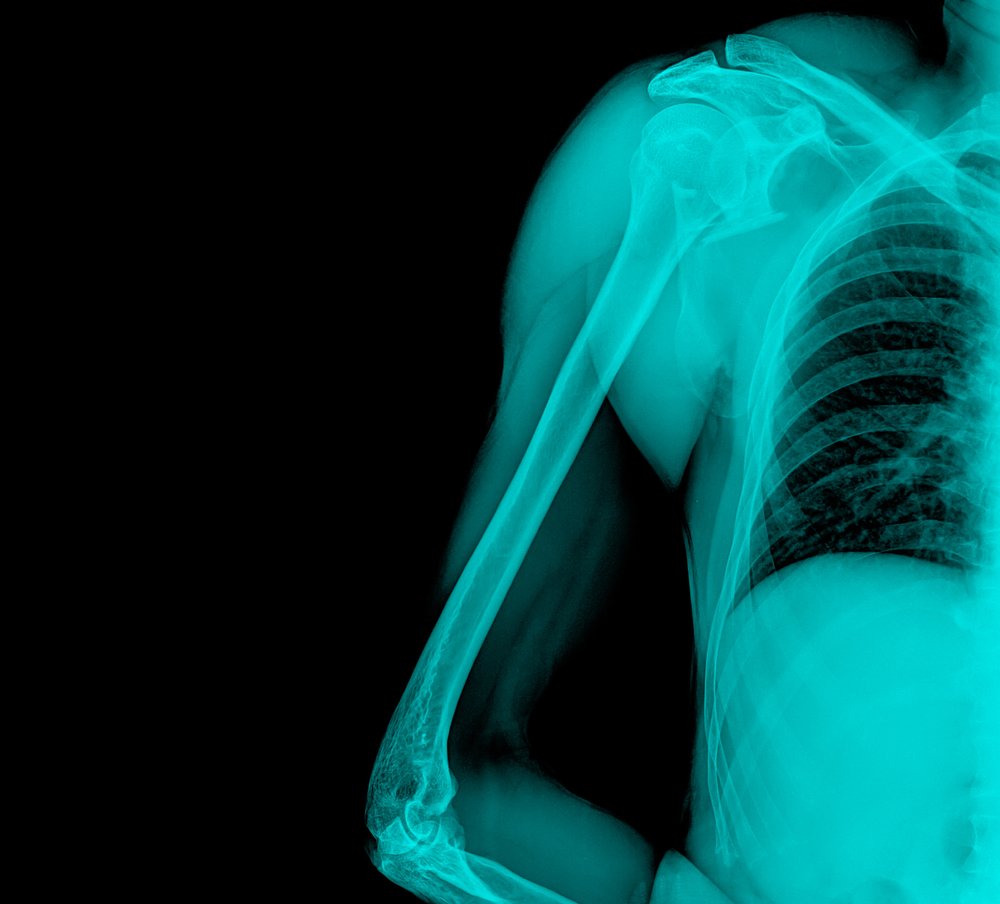
Bone symptoms are common among Gaucher patients, with problems including osteoporosis (brittle bones) and death of bone tissue due to insufficient blood supply, a condition known as avascular necrosis. It is a major irreversible complication of Gaucher disease.
While ERT is currently the standard of care for treating Gaucher patients with types 1 and 3 disease, growing evidence suggests that its effectiveness is reduced in the bone as a result of a lower uptake of the medicine by bone marrow cells.
In agreement, recent studies have reported cases of avascular necrosis despite treatment with high ERT doses.
In this study, researchers reported the case of two patients with Gaucher disease type 3 who developed avascular necrosis, despite long-term treatment with high-dose ERT. Both patients carried the most severe mutation — L483P, formerly known as L444P — in the GBA gene.
The first patient, a Hispanic male infant, was diagnosed at 14 months of age and ERT was begun at 17 months. The patient’s bone health was routinely monitored, with his bone mineral density (a measure of bone strength) being consistently below average.
He reported pain and began limping at 7 years, with scans showing signs of avascular necrosis in his femur. After performing surgery for a femur fracture, however, investigators noted improper healing and changed his ERT regimen from once-every-two-weeks to once weekly in an attempt to improve bone health.
While the surgery allowed the boy to regain full mobility at age 9, he began showing signs of postural changes by age 12, and worsening of avascular necrosis was noted one year later. By the age of 17, his visceral symptoms were stable, liver and spleen were of normal size, but his weight and height were still low for his age.
The second male patient was diagnosed at 18 months and began ERT at 22 months, which resolved his symptoms and allowed him to grow normally without signs of the condition. While clinicians detected a slightly low bone mineral density at age 11 years, the patient only developed bone symptoms by the age of 14 years.
At this point, the patient had scoliosis, but additional analysis at 16 years also revealed osteopenia (low bone density) in the lumbar spine and right hip. At 17 years, imaging tests also revealed signs of avascular necrosis in both femurs, although the patient reported no pain.
Further scans revealed below average bone mineral density of the lumbar spine, but surgery was not recommended in this case. At the age of eighteen the patient was switched from intravenous (delivered to the blood) ERT to oral substrate reduction therapy. His bone health at 20 years remained stable without evidence of bone crisis, and he continued to report no pain.
Overall, this case report suggests that ERT for Gaucher disease has limited effects in the bone marrow, highlighting the need for careful monitoring of bone health in these patients and for the development of “new treatment modalities other than ERT monotherapy to address these limitations,” researchers concluded.



