GD1 Patients Show High Prevalence of Irreversible Bone Lesions, Study Reports
Written by |
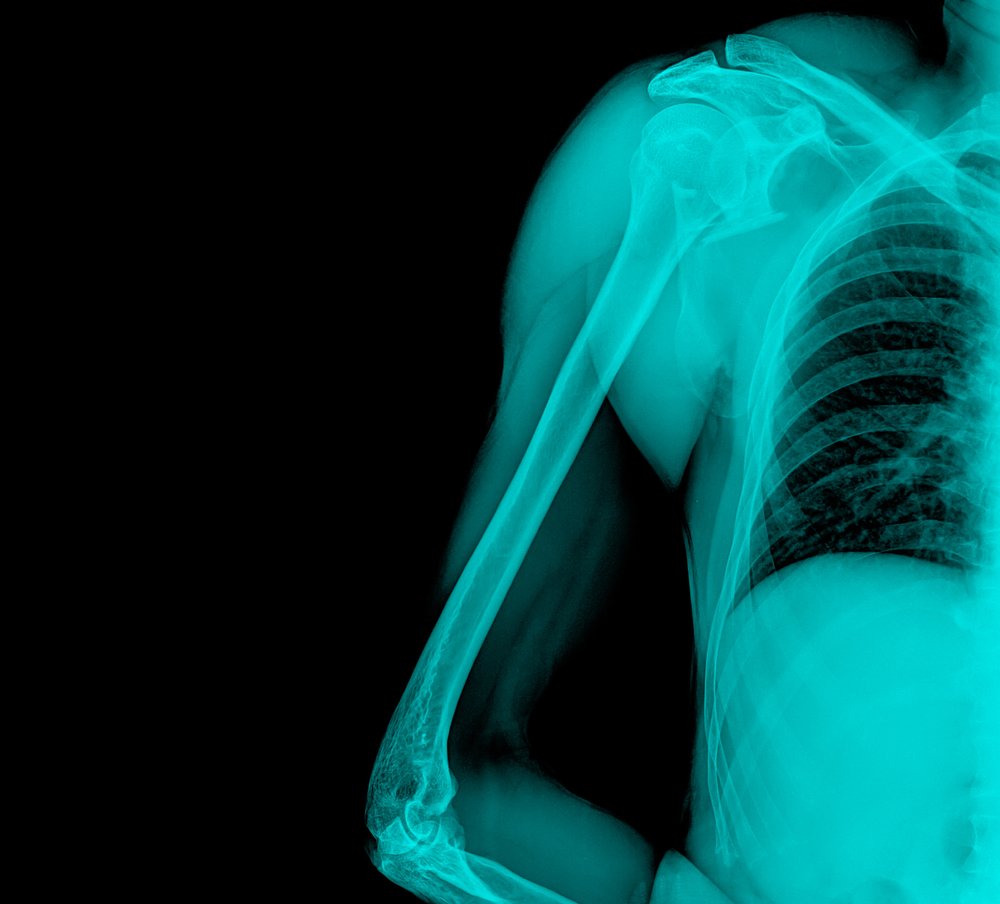
Adults with Gaucher disease type 1 (GD1) show a high prevalence of irreversible bone lesions, despite reaching treatment goals for reduced levels of blood cells, according to a study.
Findings also indicated that low bone formation, bone marrow infiltration, and spleen removal may be implicated in these lesions.
The study, “A Comprehensive Study of Bone Manifestations in Adult Patients in Argentina,” appeared in the journal Calcified Tissue International.
Given the slow skeletal response to enzyme replacement treatment and the occurrence of irreversible lesions that can affect quality of life, a thorough evaluation of bone involvement in Gaucher disease patients is necessary.
To address this, researchers described bone complications in adults with GD1 in Argentina, looking at a potential correlation between the severity of bone involvement and different parameters of bone status and Gaucher markers.
A total of 32 GD1 patients were included, all 20 years or older (mean age 40 years). All were being treated with VPRIV (velaglucerase-alfa), over a mean duration of 2.7 years. Nineteen patients had been treated with Cerezyme (imiglucerase).
Median age at diagnosis was 22 years, while mean time from diagnosis was 17.5 years.
Bone pain or bone crisis — a sudden painful event associated with signs of acute local and/or systemic inflammation — was reported by 25% of patients at the medical consultation.
A total of 90% had achieved treatment goals for low platelet counts and 94% of patients had done the same for anemia. Eight had undergone spleen removal (splenectomy). One showed a moderately enlarged liver and severe spleen enlargement.
Nine patients had a history of bone fractures, and 27 (84.4%) showed radiological changes, with a specific alteration in the femur being the most common.
Bone marrow infiltration was the most frequent anomaly found in magnetic resonance imaging (MRI), followed by irreversible lesions. Bone marrow involvement occurred in the femur of 23 patients, seven of whom also had infiltration in the lumbar spine. Marrow infiltration in the femur was significantly more common in patients with irreversible lesions than in those without these complications.
Data further showed that irreversible lesions were observed in all patients who had undergone spleen removal and in 45% of those who had not. Five of the eight patients who had undergone this surgery also showed bone marrow edema (swelling), compared with four of 22 patients who had not had their spleens removed.
Bone marrow infiltration in the femur affected all patients who underwent splenectomy, compared with 69% of the patients in the other group. The patients who underwent the surgery also had bone marrow infiltration in the lumbar spine more often (57% vs. 13%).
Only six patients had abnormal bone mineral density (BMD). Five patients older than 50 years had osteopenia — lower than normal BMD — and one had osteoporosis. Patients with a lower BMD had lower bone quality than those with higher values. Bone quality was also lower in patients who had had a splenectomy than in those who had not.
As for biomarkers, levels of 25-hydroxy-vitamin D — an indication of vitamin D levels — were insufficient in 13 patients and deficient in six patients. Parathyroid hormone levels were higher than normal in three patients, all with vitamin D deficiency.
Patients with higher levels of P1NP — a bone formation marker — had higher bone quality than those with a lower amount of P1NP. Having lower P1NP and BAP, also a bone formation marker, correlated with greater bone marrow involvement, although not statistically significant.
Even after reaching treatment goals, “a high prevalence of irreversible bone lesions was documented in this population of GD1 patients,” the researchers wrote. “Low bone formation, active bone marrow infiltration, and splenectomy might be implicated in the occurrence of [irreversible lesions].”
Of note, three of the study’s authors received honoraria from Shire.



