Researchers Identify New Therapeutic Target for Gaucher-Linked Bone Disease
Written by |
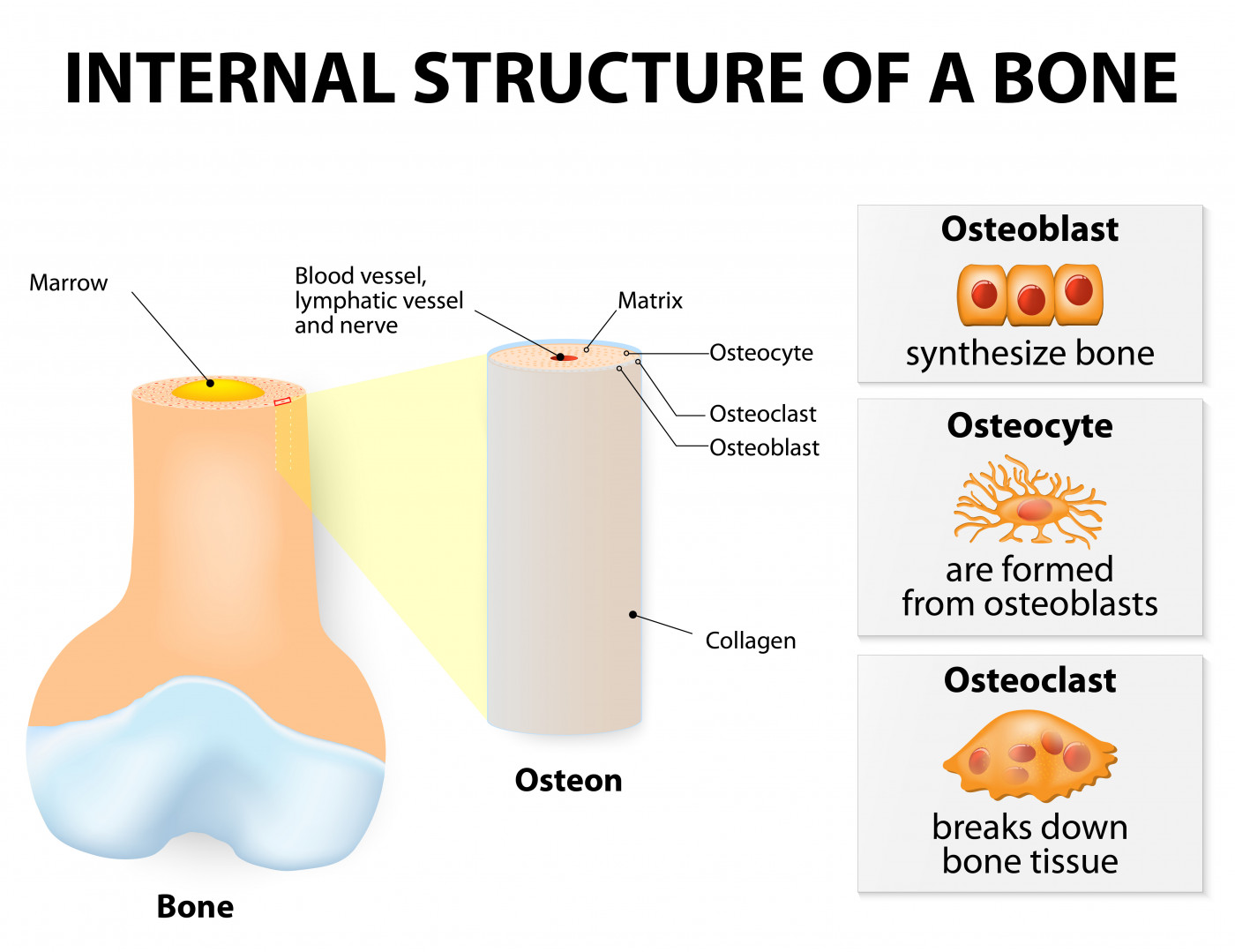
Patients with Gaucher disease (GD) frequently develop bone disease, but the mechanisms underlying bone damage remain unknown. New research points to developmental defects and impaired secretion in the cells responsible for bone formation, called osteoblasts, in all three clinical subtypes of the disease.
Particularly, researchers identified a key signaling pathway, called Wnt/beta-catenin, as a potential new therapeutic target to treat bone disease in these patients.
The study, “Gaucher disease iPSC-derived osteoblasts have developmental and lysosomal defects that impair bone matrix deposition,” was published in the journal Human Molecular Genetics.
Researchers used human induced pluripotent stem cells (iPSC) derived from patients with all three clinical subtypes of Gaucher disease – types 1, 2, and 3 – and differentiated them into osteoblasts, the cells responsible for the formation of new bone tissue. This allowed them to investigate what goes wrong in these cells in Gaucher disease.
They observed that Gaucher disease osteoblasts had developmental defects: The cells produced lower levels of several markers of osteoblast differentiation and molecules required for bone mineral formation compared to control osteoblasts. These results, researchers wrote, suggest that acid beta-glucocerebrosidase deficiency (the outcome of the mutations in the GBA1 gene and the cause of GD) “interferes with osteoblast differentiation and their bone-forming ability.”
These defects were the result of a decreased expression in the Wnt/beta-catenin pathway that has a key role in the differentiation and maturation of osteoblasts into bone-producing cells.
After adding a compound that activates Wnt/beta-catenin signaling, researchers were able to restore the developmental defects of GD osteoblasts, suggesting that not only is Wnt/beta-catenin signaling important for osteoblast maturation, it also is a potentially new therapeutic target for treating bone disease in GD.
Additionally, deposition of the bone matrix and minerals depends on the function of small intracellular organelles called lysosomes, which regulate a process called exocytosis that drives these components out of the cell. GD osteoblasts had fewer lysosomes, and lysosomal-mediated exocytosis was significantly impaired compared to control cells, the study noted.
Overall, “our results lend support to the idea that the defective phenotype of GD osteoblasts is likely to contribute to the bone manifestations observed in GD patients and animal models of GD. This study also points to the canonical Wnt signaling pathway as a novel therapeutic target to treat the skeletal abnormalities caused by GD,” the study concluded.



