Repurposed Drugs to Restore Lysosomal Acidity May Be Used to Treat Gaucher Disease
Written by |
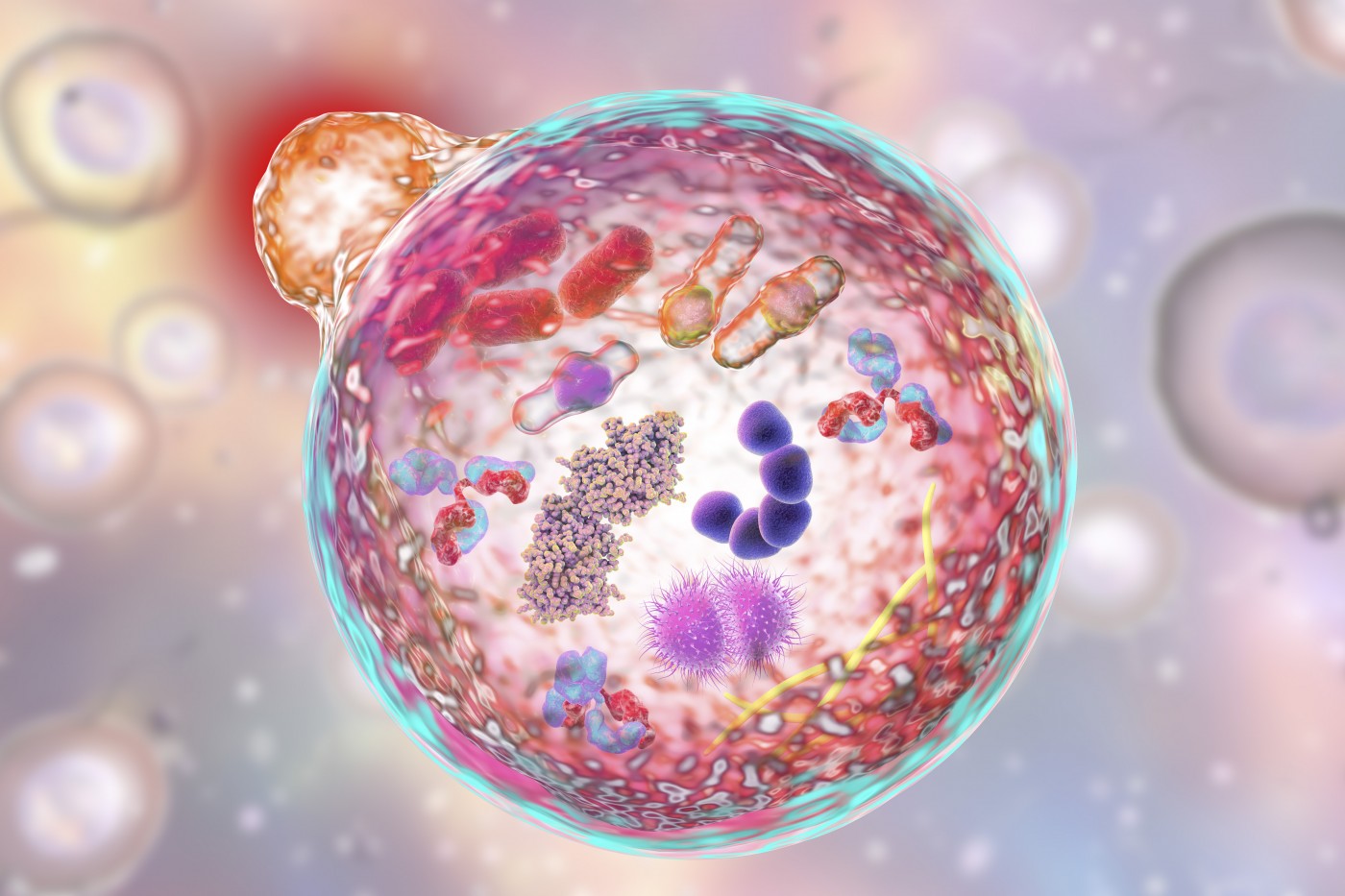
Making lysosomes more acidic may be an ingeniously simple, yet efficient, way to prevent the consequences of lysosomal storage disorders such as Gaucher disease. And restoring acidity can be achieved with repurposed drugs that are already in use for other diseases.
The discovery by researchers at the University of Rochester Medical Center is a huge step forward, as the findings can be applied to all of the about 50 different conditions caused by problems with lysosomal storage.
The study, “Lysosomal Re-acidification Prevents Lysosphingolipid-Induced Lysosomal Impairment and Cellular Toxicity,” was published in the journal PLOS Biology.
While Gaucher disease is caused by mutations in the gene coding for glucocerebrosidase, it shares a common feature with other lysosomal storage disorders. Glucocerebrosidase is an enzyme present in the lysosome — a cellular component that can be likened to the stomach. In the lysosome, molecules get churned into smaller pieces. Just like in the stomach, the environment needs to be acidic for it to work properly.
The research team discovered that the toxic buildup of substances caused by the diseases also disrupts the ability of the lysosome to keep its interior acidic. And experiments in mice showed that restoring the acidity was enough to prevent the loss of several lysosome tasks and improving cell survival.
The team then tested colforsin — a drug approved in Japan for the treatment of heart disease — in a mouse model of Krabbe disease, one of the most severe of the lysosomal storage disorders. Colforsin improved survival to the same degree as had been achieved in studies using gene therapy.
The treatment was effective even when it was started later than needed when using gene therapy, and also largely prevented brain damage. Using repurposed drugs that are already used for other conditions provides a shortcut in drug development, since the substance has already been studied extensively.
“One of the great challenges in these diseases is that they are both rare and come in many different varieties, and advances have tended to focus on single diseases,” Mark Noble, PhD, a professor of Biomedical Genetics and the study’s senior author, said in a press release.
“In contrast, our findings suggest our treatments will be relevant to multiple disorders. Also, we saw benefits of our treatment even without needing to correct the underlying genetic defects. That gives us great hope that we could combine our treatments with other candidate approaches to gain additional benefits,” Noble said.